After the transfer of an embryo, it may manage to implant in the uterus and lead to a successful pregnancy… or it may not.
The causes of this failure can be many and one of the most important is embryo quality. However, the fact that an embryo fails to implant does not necessarily mean that it is a case of what experts technically call “recurrent implantation failure (RIF)”. This is something that many people who undergo IVF treatments find difficult to understand, and it is a controversial subject.
According to the SEF (Spanish Fertility Society), there is no uniform definition for RIF. “The first definitions, which mentioned a high number of failed IVF cycles or a high number of embryos transferred, have become obsolete thanks to better embryo selection and technological advances,” explains Dr Dalia Rodríguez, a fertility specialist at Dexeus Mujer.
The most recent consensus definition is the one agreed upon by the members of the “Lugano Workshop”, with the contribution of 27 international experts, explains Dr Marta Devesa, a fertility specialist at Dexeus Mujer. According to this group of experts, recurrent implantation failure is described as “the absence of clinical pregnancy after the transfer of at least three euploid embryos (without chromosomal abnormalities) in women who do not present a uterine problem”, or “after the transfer of the number of embryos considered sufficient and appropriate to the age of each woman, if these have not been genetically analysed”, she points out.
To better understand why diagnosing and defining RIF is complex, it is important to consider several aspects:
- Getting pregnant is not as easy as it seems, even naturally. The chances of achieving a pregnancy for a young couple without fertility problems who have regular sexual intercourse and do not use any contraceptive methods are only 25%. Moreover, that is assuming that both are in good health, that the woman is under 38 years of age and that there are no incompatibility problems or other genetic abnormalities.
- Most of the patients who resort to our Fertility Unit already have trouble conceiving, so it is necessary to accept that it is possible not to achieve a pregnancy at the first attempt and sometimes not even after the second attempt.
- Not all embryos succeed in developing, even if they appear to be of good quality. That being said, it is true that in fertility treatments, the transfer is carried out at the right time, so in theory, there is a better chance that it will work.
- Further testing to find out what went wrong is not always helpful. A person with fertility problems may have had several failed treatments and wonder if there is an additional problem, not known or previously undetected in the basic tests, that is preventing a pregnancy. But this does not systematically mean that there is an implantation failure, nor that it is necessary to start performing additional tests to detect what is wrong. In fact, it is important to note that there is very little evidence about the usefulness of many of the tests offered to patients after an IVF failure.
After all these explanations, the question is: what protocol should be followed in these cases?
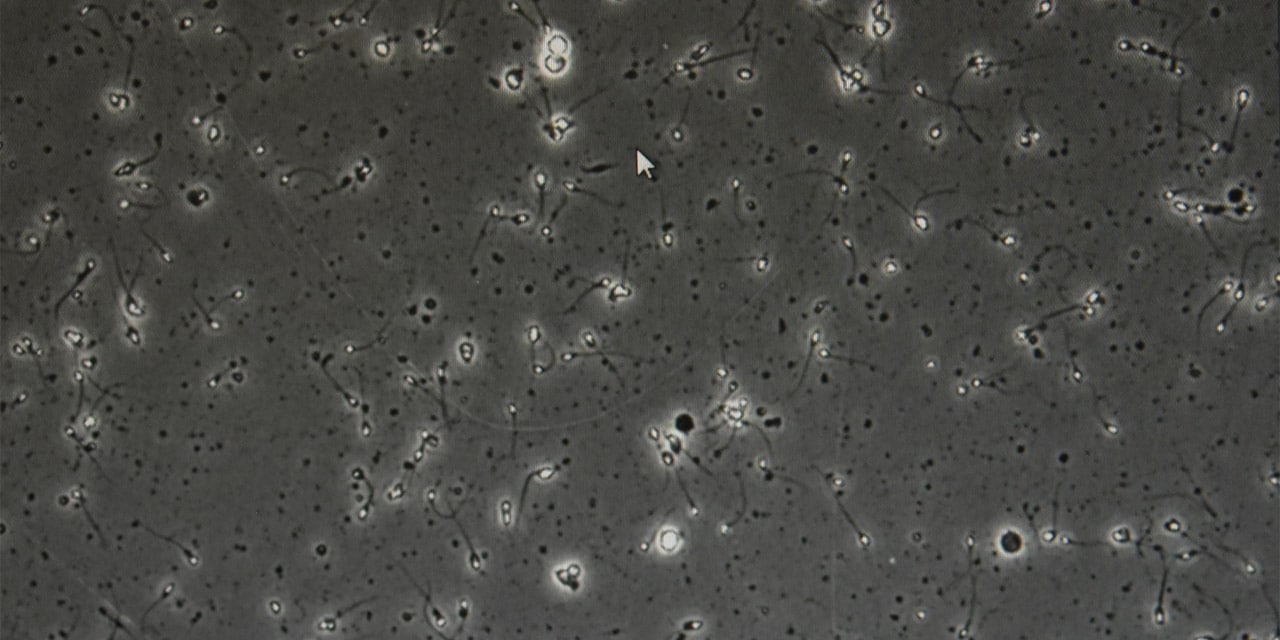
“The embryonic chromosomal factor is very important because that is the main reason why an embryo fails to implant. That is why in women aged 39 or older, where the rate of embryonic chromosomal abnormalities begins to increase due to age alone, we recommend carrying out an IVF cycle with genetic screening of the embryo before transferring it into the uterus: PGT-A”, adds Dr Devesa.
Another factor to consider is the uterine cavity, which is why it is advisable to carry out an ultrasound scan, ideally with a 3D capture of the cavity. In this case, the goal is to rule out uterine malformations or pathologies such as myomas, which may affect the cavity, polyps, adhesions, adenomyosis (presence of endometrial tissue in the uterine muscular layer) and other alterations.
Other tests that can also be performed are a hysteroscopy and an endometrial biopsy to detect whether there are certain functional abnormalities in the endometrium, such as alterations of the microbiota, endometriosis or endometritis, among others.
On the other hand, some specific conditions in women, such as endocrine disorders, hypothyroidism, hyperthyroidism and other autoimmune disorders can have a negative impact on implantation..
“Our position in these cases is to support our patients and offer them all the help available to improve the results while assessing the effectiveness and usefulness of each step, without overdiagnosing or prescribing additional treatments if it is not necessary,” says Dr Devesa. “We should always be prudent in this regard, and if we prescribe an additional treatment, we should make it clear that these are measures which may be beneficial but are not a guarantee that the patients will achieve their goal.
In these cases of recurrent failures, “professionals sometimes refer patients to specialists in endocrinology, if they consider it necessary, or advise them to request a consultation with the Haematology or Immunology Unit when they suspect there may be an autoimmune pathology or a haematological problem,” says Dr Dalia Rodríguez. “We also advise them to visit our Nutrition Unit, as more and more importance is being given to lifestyle and fertility,” she adds.
By way of conclusion: not achieving a pregnancy after transferring one or two embryos does not imply a recurrent implantation failure. We must be prudent when it comes to the additional tests and treatments prescribed, many of which are costly and not without side effects. It is essential to offer patients and their partners the possibility of receiving emotional support during the process, in case they need it, as it is not easy to accept several reproductive failures, nor to try again without doing “anything new” to help understand why the first attempts did not succeed. or to have the hope that future attempts can be successful.
If you have experienced more than one reproductive failure, don’t jump to conclusions or be disappointed. Talk to your gynaecologist and let them guide you.