Polycystic ovary syndrome (PCOS) is not a fertility problem per se, but it can lead to irregular cycles or a lack of ovulation. It is caused by an imbalance in the hormones responsible for regulating the menstrual cycle, resulting in impaired ovulation, which can make it more difficult to become pregnant.
In addition, it is a multifactorial disorder that can lead to the development of diabetes and obesity, two health issues that also have a negative impact on fertility and can have repercussions on a woman’s potential pregnancy and overall health. However, not all women who suffer from it have the same symptoms. This is why each case should be individually assessed.
In this post, Dr Ainhoa Coco, a gynaecologist specialising in endocrinology and reproductive medicine at Dexeus Mujer, answers some frequently asked questions on this subject.
What percentage of women who suffer from this syndrome can have or do have fertility problems?
Polycystic ovary syndrome (PCOS) is one of the most common and heterogeneous endocrine, reproductive and metabolic conditions. Its prevalence ranges from 4 to 21% worldwide – depending on the criteria used – and it is the leading cause of infertility due to lack of ovulation. The impact of PCOS on fertility cannot be generalised, but it is always an issue that needs to be considered. However, there is no need to worry prematurely, as having PCOS does not necessarily mean that you will have difficulty getting pregnant.
But is it possible to get pregnant naturally?
Yes, because not every woman experiences the same symptoms and if ovulation occurs, even if not regularly, the egg can be fertilised. However, PCOS also affects the production of oestrogen and progesterone, two hormones that increase endometrial receptivity. Therefore, even if ovulation occurs and the egg is fertilised, it may be more difficult for the embryo to implant, thrive and result in a pregnancy.
And if there are any problems, is it necessary to resort to assisted reproduction techniques?
As we have already mentioned, each case must be assessed individually, because the symptoms can be very different from one woman to another. The first line of treatment for PCOS is a healthy lifestyle, which includes nutritional strategies, physical activity, good rest, etc. All of this with the aim of restoring spontaneous ovulation. If, despite this, spontaneous ovulation is not achieved, there are different ovulation-inducing treatments.
If the problem is anovulation and there are no other sterility factors, the doctor may recommend a treatment to induce ovulation and, depending on the results, decide whether it is necessary to resort to more complex techniques. In any case, it is also very important to approach the problem from a multidisciplinary perspective in order to improve your lifestyle: small strategies not only help improve pregnancy rates but also help you be in the best possible condition to carry out a pregnancy, as this has an impact on your overall health, as well as that of your future baby.
When is in vitro fertilisation (IVF) indicated?
IVF may be an option if you wish to become a mother, provided that you have tried to change your habits without any improvement and that the medication prescribed by your doctor has not been effective. IVF is the most complex fertility treatment, but also the one with the highest success rates, so each case must be individualised, taking into account the context of each patient and other additional factors such as age, whether there is an additional fertility problem in the couple, etc., to decide which is the best option.
If a patient with PCOS undergoes a fertility treatment, does she have more risks than a woman who does not suffer from this disease?
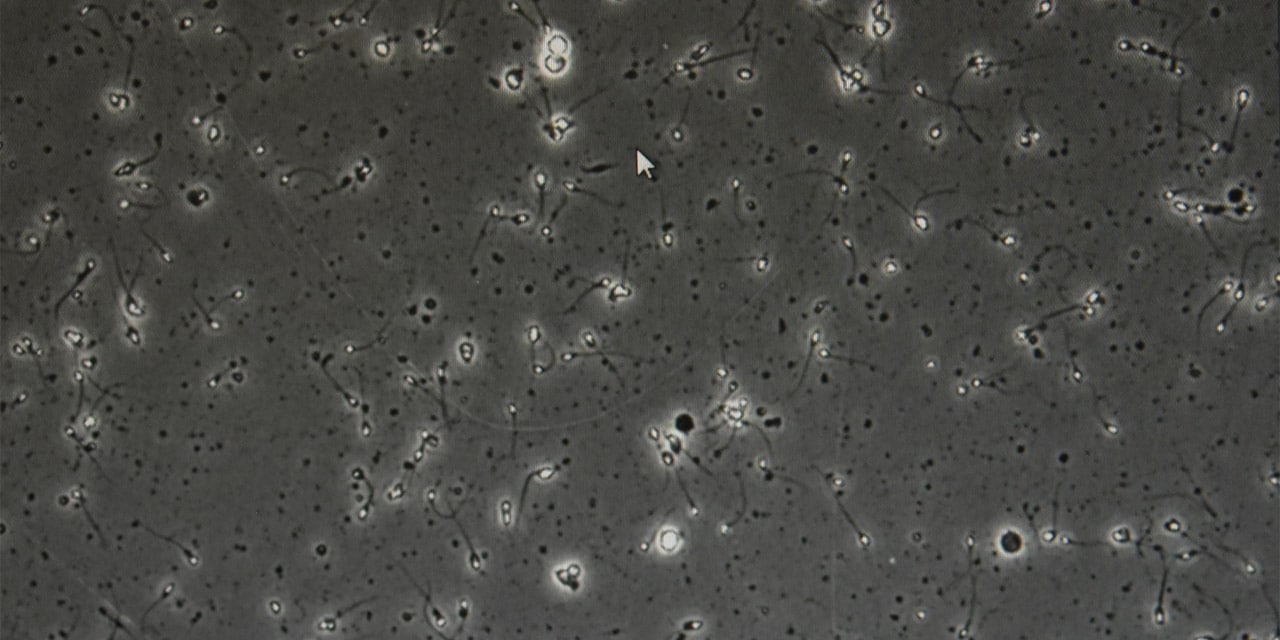
Women with PCOS have a high number of antral follicles. These are small sacs of fluid found in the ovaries, which appear at the beginning of each menstrual cycle and contain immature eggs. Each menstrual cycle, the ovaries recruit several antral follicles, i.e. they select a group of eggs. This is why it is important for women with PCOS undergoing hormonal ovarian stimulation treatment to monitor the process more closely and thoroughly to avoid hyperstimulation.
In any case, nowadays, hyperstimulation is rare, as there are already measures in place to prevent this from happening, so we can confidently say that IVF is a safe treatment even with PCOS.
Is there also an increased risk of complications during pregnancy?
It seems that women with polycystic ovary syndrome (PCOS) have a higher risk of suffering certain problems or complications during pregnancy, such as premature delivery, excessive weight gain during pregnancy, hypertension, gestational diabetes or pre-eclampsia (a cardiovascular disorder that can affect both the mother’s and the baby’s health). At our centre, we have a Unit specialised in the diagnosis and treatment of Polycystic Ovary Syndrome and a High-Risk Pregnancy Unit as well as a Pre-pregnancy Counseling Unit that work in coordination with the Reproductive Medicine Department, which facilitates the monitoring and care of patients with PCOS who wish to become pregnant. In addition, as already mentioned, it is important to adopt a multidisciplinary approach and to ensure good metabolic control regardless of whether or not you are trying to become pregnant, so if you think you may have PCOS, do not hesitate to consult us.