Due to their ability to continue producing new sperm, men remain fertile for longer than women. However, studies show that the sperm produced by men around the age of 60 does not have the same fertility potential as that of a 25-year-old, because from the age of 45 onward, the potential for fertilisation and conception through intercourse is reduced.
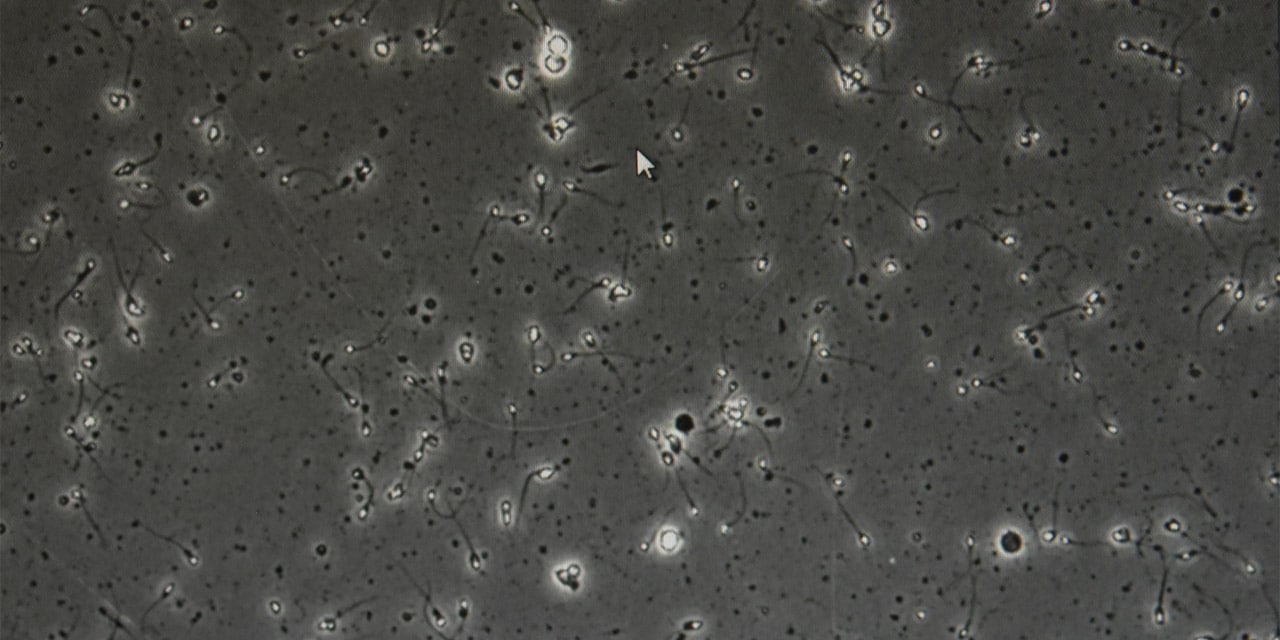
So how does ageing affect male fertility? For starters, it has been shown to affect the production of hormones and sperm, and while there is still much to investigate, available data and results show that as with any other cell in the body, the ageing process can alter spermatozoa at the molecular level and hence impair sperm function.
Sperm ageing is the result of complex interactions between molecular damage, maintenance and repair within the testes. It is an irreversible process which can be influenced by lifestyle and genetics. The sperm of older men is therefore more likely to present morphological alterations and de novo (i.e. non-hereditary) genetic mutations in the offspring, which has also been associated with the development of neurocognitive disorders.
It is therefore essential that men over the age of 45 years who wish to conceive request an assessment by an andrology expert, as the risk of certain multifactor malformations in the offspring is significant when the father is over 50. In fact, many miscarriages and problems conceiving in older couples are due precisely to genetic alterations that hinder the development of the embryo, and we now know that the male factor plays a significant role in this regard.
In any case, age-related infertility is a problem which is set to increase in developed societies, just like delayed fatherhood. For this reason, although there is much talk of delayed motherhood, it is important to know that male fertility also has its limits, and that becoming a father at 50 is not only more tiring than at 30, but also more difficult.